Most women experience pelvic pain at times. Over 700,000 Australian women have endometriosis; could you be one of them?
To mark Endometriosis Awareness Month (March), here’s a quick wrap-up of what we know (and don’t know) about endo.
What is endometriosis?
The simplest explanation for endometriosis is that tissue similar to the lining of the uterus (endometrium) is present in other parts of the body, commonly the pelvis. We think it gets there largely by a process called “retrograde menstruation”, where the menstrual blood leaks back up the fallopian tubes and enters the pelvis instead of just draining out vaginally. Once in the pelvis it can attach there as “lesions” which are affected by hormonal cycles and can cause long-term problems. The full explanation is a lot more complicated than this however, and poorly understood. For example, endo has been found in parts of the body that could not POSSIBLY be explained this way.
How does endometriosis cause pain?
When this endometrial-type tissue is present in the pelvis it causes irritation and pain. Sometimes it causes the sticking-together (“adhesion”) of structures within the pelvis such as the uterus, bowel, bladder, ovaries and fallopian tubes. Endo or adhesions may interfere with the normal functioning of these organs or cause pain during activities like defecation, urination and intercourse. Endometrial deposits called adenomyosis can also be present within the muscular wall of the uterus. When the lining of the uterus sheds every month, adenomyosis also secretes into the uterine wall causing distention and pain.
How does endometriosis affect fertility?
Endo is toxic to eggs released by the ovaries at ovulation. It can also cause blockage of the fallopian tubes, contributing to the infertility experienced by many women. Cysts called endometriomas or “chocolate cysts” filled with blood may form on the ovaries and interfere with ovulation. Another huge barrier to conception is sexual pain, which discourages women from having intercourse at all.
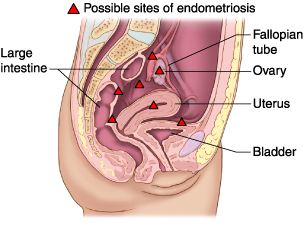 Image courtesy of MDguidelines.com
Image courtesy of MDguidelines.comHow is endometriosis diagnosed?
If you are experiencing pelvic pain or infertility your GP should be the first port of call. A detailed pain and menstrual history should help to distinguish between endometriosis and other possible causes of your symptoms. There will usually be some tests involved as well, including blood tests and a vaginal ultrasound scan. Expert ultrasound is a great non-invasive choice for the diagnosis and staging of endometriosis. Unfortunately it is only available from a limited number of operators who are specially trained to detect the subtle signs. Laparoscopic (keyhole) surgery is the definitive way to find endo but should be avoided for diagnosis if possible. Women with severe endo and/ or fertility problems can end up having many surgeries in their lifetime, each with it’s own risk and complications. Ideally the first surgery should be planned carefully by a specialist surgeon who can also treat whatever they find at the same time.
How is endometriosis treated?
Endometriosis is a chronic disease affecting women in a variety of ways over a long period of time, sometimes beginning in their teens. The pain and infertility it causes can impact in all areas of a woman’s life: her ability to work, exercise or care for herself and her family. Also her relationships, her sexuality, even her mental health and self-esteem can be affected. We now realise the importance of multidisciplinary care and self-management strategies in dealing holistically with endo. To facilitate multidisciplinary care an endometriosis treatment plan may include these healthcare providers:
- General Practitioner (GP)- It is crucial for women with endo to have a good relationship with a doctor who can initiate first-line medical treatments, coordinate overall care, collate results and make appropriate referrals. GP’s can also work with you to produce a Chronic Disease Care Plan which outlines the role of each care team member. These are Medicare-rebateable and usually bulk-billed.
- Physiotherapist- The importance of a good pelvic floor physiotherapist cannot be overstated. Women with endo may have pain with penetration (perhaps even tampon use), intercourse, defecation, urination, or even just sitting and moving about. A good pelvic floor physio can assess and diagnose these problems and teach techniques that reduce pain. Targeted daily stretching and exercises can make a huge difference to pelvic pain.
- Psychologist or counsellor- Women with endo may experience a variety of emotional reactions: grief, anger, frustration, despondency, anxiety and depression among them. They may also experience relationship problems caused by chronic mental health or intimacy problems, even fearing to cuddle or kiss their partner in case it leads to sex (pain!). Individual or couple’s counselling may be appropriate in these circumstances.
- Gynaecologist- Most women with endo will visit a gynaecologist at some point, either for an advanced diagnostic ultrasound, initiation of medical treatment or surgical intervention. Not all gynaecologists perform laparoscopic surgery, and those that do require higher level qualifications to deal with advanced endometriosis, so get your GP to ensure an appropriate referral.
Other allied health and complementary therapists can also be included as appropriate, eg. dieticians, masseuses, acupuncturists, yoga instructors, etc.
What causes Chronic Pelvic Pain (CPP)?
The keynote speaker at Canberra’s ‘Illuminating Endometriosis’ seminar in 2016, Dr Susan Evans, explained that endo is just one mechanism for the development of Chronic Pelvic Pain (CPP). Other causes of pelvic pain may co-exist with endo and also send pain signals to the brain: pelvic muscle spasms, bladder or bowel problems, vulval or vaginal conditions, injuries and sexual trauma. These pain signals get larger and stronger with constant or repeated pain exposure over time. Women can gradually become hypersensitive to pain, so that eventually even the most minor, non-painful stimulus is perceived by the brain as being painful. Thankfully this process can also be gradually reversed, or “down-regulated” with the right treatment. This is where the strategy of self-management becomes all-important.
The importance of self-management in endometriosis
To tackle endo head-on women must be empowered by knowledge: knowledge about themselves and their own bodies as well as knowledge of the disease. Women must individually explore what works best for them to:
- manage their pain,
- maintain optimal health,
- gain best possible quality of life every day, and
- maintain great relationships.
Sufferers also need to consider and explore other possible causes of pain that may exist concurrently with their endo. For effective self-management women must feel empowered to seek out the information and support they need. By building and accessing support networks, women with endometriosis can connect with the experiences of others and share knowledge.
Links and resources
- Endometriosis Australia
- The National Action Plan for Endometriosis
- Jean Hailes for Women’s Health
- Book: “Endometriosis and Pelvic Pain”, by Dr Susan Evans. A great step-by-step walk through the various aspects of endo and pelvic pain…. an absolute must-read for any woman with endometriosis or chronic pain.
- The Pelvic Pain foundation of Australia: A not-for-profit organisation that promotes information and events about pelvic pain. This site has loads of detailed information about endo including treatment options.
- EndoActive: Online information, support and a facebook community
What is WellFemme About?
If you can’t find the professional help you need for your peri/menopausal symptoms then book a Telehealth consultation with an expert WellFemme menopause doctor.
WellFemme is Australia’s first dedicated Telehealth menopause clinic, servicing locations nationwide including: Melbourne, Sydney, Adelaide, Darwin, Perth, Hobart, Brisbane, Dubbo, Bendigo, Broken Hill, Broome, Alice Springs, Launceston, Cairns, Mildura, Lightning Ridge, Kalgoorlie, Albany, Toowoomba, Charleville, Port Headland, Katherine, Ballarat, Coober Pedy, Bourke, Albury… and your place!
Tags
endometriosis, how is endometriosis diagnosed, how to treat endometriosis, infertility, pelvic pain, what causes endometriosis, what causes pelvic pain, what is endometriosis,

