The Senate Committee Inquiry into Peri/menopause generated 25 key recommendations, but it will all come to nothing if Government won’t commit to act on them. Here’s how YOU can help ensure that they do!
The Senate Committee members worked their way through 285 submissions and 7 hearings with 118 witnesses this year, and handed down a comprehensive set of recommendations last month. The government now has 3 months to respond, and there are no guarantees that they will accept these recommendations or act on them.
The other wildcard here is the 2025 election; what if government commits to the recommendations, but then there is a change of government?
Last week Senator Larissa Waters proudly announced the Greens’ plan to allocate $50M annually to peri and menopause related improvements from the Committee’s recommendations. We now need to put pressure on both the government and opposition to at least match- if not exceed- the Greens’ commitment.
This is where YOU can really make a difference. We have provided a draft email below that you can send to the government, opposition and your local MP requesting their commitment to the Senate Committee’s recommendations.
We urge you to please take 5 minutes to send this email, and copy in your local MP. It’s a small but powerful gesture that might make all the difference to services, treatments and conditions for present and future generations of peri and menopausal women.
OUR SUGGESTED EMAIL TO SEND YOUR GOVERNMENT, OPPOSITION AND LOCAL MEMBERS:
TO: Mark.Butler.MP@aph.gov.au, Ged.Kearney.MP@aph.gov.au, Senator.Ruston@aph.gov.au, Sussan.Ley.MP@aph.gov.au, [Your local MP’s email]
Dear [Minister/Senator/MP],
As a constituent I want to bring to your attention an issue I want more action on: perimenopause and menopause.
Too many women have suffered in silence due to:
- gender bias in our health system,
- a lack of information about peri and menopause, and
- a lack of affordable treatments.
Last month, all parties came together to support 25 key recommendations on perimenopause and menopause. You can read the full report here.
I want to see these recommendations implemented in full and I want this to be an election issue.
Now is the time for action. Women deserve better, and I want to make sure our voices are heard.
The Greens are committed to addressing all the recommendations from the Senate inquiry and allocating $50M per year for that purpose; I am calling on you to match this commitment.
I’d also like the opportunity to speak to you more about [xxxx]
Kind Regards, [Name and signature]
Read Dr Kelly Teagle’s Senate Inquiry submission HERE
View Dr Kelly Teagle’s response to the Senate Committee’s recommendations on Instagram HERE
What is WellFemme About?
If you can’t find the professional help you need for your menopause or perimenopausal symptoms then book a Telehealth consultation with an expert WellFemme menopause doctor.
Tags
Australian Senate menopause inquiry., Menopause senate inquiry, Parliamentary Senate Inquiry, Senate Inquiry Menopause, Senate Inquiry Perimenopause,
WellFemme founder Dr Kelly Teagle has made the following submission to the upcoming Senate Inquiry into menopause:
Committee Secretary
Community Affairs Committee
Department of the Senate
PO Box 6100
Parliament House
CANBERRA ACT 2600
AUSTRALIA
Dr Kelly Teagle, MBBS, BSc, FRACGP, Grad Dip Women’s Health
Principal clinician, WellFemme Telehealth menopause clinic
14th March, 2024
Submission to the Standing Committee on Community Affairs, Inquiry into issues related to menopause and perimenopause.
To the Senate Inquiry Committee,
Thank you for the opportunity to make a submission to this inquiry. I am Dr Kelly Teagle, a GP specialising in menopause and founder of the WellFemme Telehealth menopause clinic in 2018. WellFemme now has 18 doctors and thousands of patients Australia wide, and demand is growing.
Executive Summary of Recommendations
I wish to make the following recommendations for the Committee to consider:
(As per Annex A):
- Ensure that the safest evidence-based treatments are listed on the PBS.
- Create a well-rebated, long consult Medicare item for thorough perimenopausal assessments.
- Provide funding for the Australasian Menopause Society to oversee GP menopause training.
- Support GP’s at point-of-care through a combination of rapid-access specialist advice, clinical software algorithms and streamlined referral pathways.
- Ensure that GPs are well remunerated under Medicare for longer consultations.
- Permanently include Telehealth items for reproductive and sexual health care in the MBS.
- Design and deliver public awareness campaigns which are accessible and easily understood regardless of education, language, gender identity, culture or disability.
- Develop and maintain a DHAC website which collates all the best menopause resources for GP’s and consumers in one well-publicised, up to date location. Include infographics and videos which are translated and adapted for various vulnerable consumer populations.
Additionally:
- Develop a National Menopause Action Plan with input from key service and policy stakeholders, and
- Conduct a review of how menopause (and women’s health related) projects are funded.
I would like to comment particularly on sections b, f, h and i of the terms of reference:
b. The physical health impacts, including menopausal and perimenopausal symptoms, associated medical conditions such as menorrhagia, and access to healthcare services;
As a GP I have specialised in menopause care for over a decade now. Personally, I experienced a very early and highly symptomatic menopause at age 42 and had breast cancer in 2022. My perspectives on menopause come from a combination of personal and clinical experiences and my professional knowledge base.
Australian data from 2016 indicated that close to 400 000 women were experiencing untreated moderate to severe hot flushes and night sweats, and this just one symptom of the menopausal transition. For the 15-20% of women with severe symptoms it impacts their ability to sleep, think, work, and interact with loved ones. It erodes functioning, mood, self-confidence and quality of life.
I spoke about some of the reasons why women are not accessing appropriate treatments in an award-winning address to the 2022 Successes and Failures in Telehealth Conference: “Barriers and Breakthroughs in Tele-menopause Care.” [Slides available HERE]
In my presentation to the 2023 Parliamentary Round Table on menopause I also spoke specifically about the problems of access to services; my recommendations are detailed in this link and the 2-page summary at Annex A.
f. The level of awareness amongst medical professionals and patients of the symptoms of menopause and perimenopause and the treatments, including the affordability and availability of treatments;
Telehealth is not just good for clinician-to-patient services; there is untapped potential for its use in clinician-to-clinician support. Non-specialist GP’s who might avoid treating their menopausal patients due to a lack of professional expertise or confidence could discuss their cases with more specialised doctors by phone or video.
Outreach models that support GP’s in managing their own patients locally will help keep menopause management in primary care whilst supporting and upskilling GP’s wherever they are. WellFemme is uniquely experienced and resourced with expert menopause clinicians to assist governments in the delivery of such a service.
Telehealth delivery of menopause care has been well validated over almost 5 years of WellFemme operations, and demand for services continues to grow. As outlined in this presentation, service uptake increased dramatically due to COVID and the advent of Telehealth Medicare rebates. To ensure ongoing access to menopause care for ALL Australians who need it, permanent inclusion of Medicare rebates for Telehealth provision of reproductive and sexual health services is essential.
Regarding affordability of best evidence-based treatments: micronized (body-identical) progesterone has overwhelmingly proven to be the safest progestogen for MHT, but it is not subsidised under the PBS. Financially vulnerable women must instead settle for cheaper synthetic progestins that have been shown to increase breast cancer risk.
Additionally, rebates for longer consultations (as needed to properly manage menopausal patients) should reimburse patients at the same cost-per-minute rate as shorter consultations. This is crucial to incentivise GPs to conduct preventive healthcare activities. Medicare inequities also worsen the GP gender pay gap as female GP’s do many more long consultations than males, particularly for complex conditions and mental health care.
h. Existing Commonwealth, state and territory government policies, programs, and healthcare initiatives addressing menopause and perimenopause;
Roles and scope of the many (and growing) organisations in the menopause space are not clearly defined. A comprehensive approach to improving community health and wellbeing will require a strategic model with clearly allocated roles and funding for the various stakeholders, such as those involved in:
- Policy development and provision of advice to government
- Design and execution of research
- Examination and interpretation of evidence for clinicians and the public
- Development and delivery of clinical education to health professionals
- Design and delivery of public awareness campaigns and a definitive website
- Development of networked systems to support GP’s in their local communities
- Development and execution of an integrated national plan for service delivery to public patients utilising a combination of Telehealth and in-clinic options.
- Facilitating and overseeing the supply of affordable, evidence-based medications
For example, the Australasian Menopause Society is Australia’s premier organisation for the collation of worldwide evidence and provision of evidence- based resources for clinicians and consumers. They have neither the resources or funding to develop and deliver formal GP education programs, but they certainly would be the logical organisation to oversee accreditation standards for GP menopause education programs that might be developed by third party providers. This would require consultation with government and allocation of resources and funding for the AMS to take on such a role.
As recommended at the 2023 Parliamentary Round Table, the best (and most cost-effective) way to bring stakeholders together to map out these strategies is to develop a National Menopause Action Plan.
i. How other jurisdictions support individuals experiencing menopause and peri-menopause from a health and workplace policy perspective; and any other related matter.
Most menopause stakeholders have no visibility of government processes for identifying and funding priority peri/ menopause related projects, or their associated tender opportunities. I recommend a review of how such projects are conducted, with clear communication to all potential stakeholders about what work is needed and how to tender or apply for it.
I have contributed to a separate joint submission with A/Prof Erin Morton on this topic.
Yours Sincerely,
Dr Kelly Teagle
References: As hyperlinked throughout
Annex A to Senate Inquiry submission 2024 Dr Kelly Teagle
What is WellFemme About?
If you can’t find the professional help you need for your menopause or perimenopausal symptoms then book a Telehealth consultation with an expert WellFemme menopause doctor.
Tags
Australian Senate menopause inquiry., Menopause senate inquiry, Parliamentary Senate Inquiry, Senate Inquiry Menopause, Senate Inquiry Perimenopause,
In an unprecedented event, Parliament House rang with voices calling for reform in Australia’s approach to the menopausal transition.
PHOTO ABOVE, L to R: Peta Murphy MP, Prof Jayashri Kulkarni, Sen. Hon Anne Ruston, Prof Rod Baber, Dr Karen Magraith, Dr Kelly Teagle, Shelly Horton, Dr Ginni Mansberg, Hon Ged Kearney MP, Prof Sue Davis, Bridget Archer MP, Hon Emma McBride MP.

Front, L to R: Researcher Erin Morton, TV journalist Shelly Horton, Prof Jayashri Kulkarni and MP Peta Murphy with the team of menopause experts and advocates.
7th March 2023 was a landmark day in Parliament House: the #MenopauseMatters Parliamentary Round Table was the first time that menopause had been formally presented in those hallowed (predominantly male) halls. We had it all: flooding periods, tears, VAGINAS (![]() )… and that was just the politicians’ speeches!
)… and that was just the politicians’ speeches!
Our consortium of menopause experts gave (to quote several Ministerial attendees) “the best Round Table presentation I’ve ever attended”. The speakers were united in calling for development of a National Menopause Action Plan, to consolidate all the expert recommendations and formally incorporate them into Government policy.
We can’t rest on our laurels though; you can help keep the pressure on by asking your local MP to support the push for a National Menopause Action Plan… tell them loud and clear that MENOPAUSE MATTERS!
The following is from the written submission to the Round Table by WellFemme Founder Dr Kelly Teagle:
EMPOWERMENT during the menopausal transition: equitable access to information, services and treatments
Menopause is not a disease. The menopausal transition is a life-stage experienced by half the population which lasts for decades, with physiological changes that significantly impact future health. Many people experience debilitating symptoms which can be managed with the right information and support.
The Scope of the Problem
In 2016 an Australian research group, including Prof Sue Davis, estimated that almost 400 000 Australian women were needlessly suffering with untreated flushes and sweats; and this is just one symptom of the many symptoms of the menopausal transition.
Why aren’t women getting the help they need in the menopausal transition?
This is an excellent question which is also currently being examined by Minister Kearney’s National Women’s Health Advisory Council.
Individual barriers to Equitable Service Access
- There’s poor general public awareness of how early and long the menopausal transition can be, it’s functional impact and the availability of safe, effective treatments.
- Women may avoid seeking treatment due to lingering fears about the safety of hormonal treatments; these are in fact well established to be safe and effective for most symptomatic women.
- Some women are particularly vulnerable due to cultural barriers, disability, poor education, low income or lack of social supports, making it even harder to access information and services.
- Women who have been dismissed, misdiagnosed, over-investigated and poorly treated by doctors may give up trying to get help for fear of further frustration and humiliation.
- Financially disadvantaged patients often have to accept cheaper, potentially riskier hormonal products. Evidence suggests that certain hormonal treatments are safer choices, but these are not covered by the Pharmaceutical Benefits Scheme.
Barriers to Equitable service access in Primary Care
- There is a nationwide GP shortage, worst in the rural and remote areas. Women struggle to access ANY GP, let alone finding one who is knowledgeable and approachable about peri/menopausal issues.
- Rural GPs are often transient locums, or from non-English speaking backgrounds, so there may be language, gender or cultural barriers to menopause discussions with their patients.
- Women avoid seeing a GP they don’t feel comfortable with, leaving them desperate for options. They often resort to unproven and potentially harmful (but easily purchased) products and services.
- GP’s often lack training and confidence about menopause treatments and may be completely unaware that perimenopause even exists, leading them to be dismissive of symptoms or avoid discussions.
- GP’s who do treat peri/menopausal patients are financially disadvantaged under Medicare for the longer consultations needed to make thorough assessments and management plans.
Opportunities and Innovative Solutions
Women are desperate for information and support, as evidenced by the huge growth of online support groups, such as Menopause and Perimenopause Support Group on Facebook which has over 24 000 members.
The pandemic forced a rapid adaptation to Telehealth, which has now been well validated for medical service delivery over several years in Australia. The creation of new Medicare rebates specifically for reproductive and sexual health care in 2021 was pivotal in removing barriers related to privacy or locality. WellFemme, a solely Telehealth menopause clinic founded in 2019, has experienced a steady increase in demand for services and now helps thousands of women all over Australia.
A Targeted Approach to Achieve Equitable Access to Information, Services and Treatment
To improve access for financially disadvantaged people:
- Ensure that the safest evidence-based preparations are listed on the Pharmaceutical Benefits Scheme
- Create a well-rebated, long consult Medicare item for thorough perimenopausal assessments; this could be achieved through inclusion in the current Health Assessment items (eg. 705)
To facilitate good menopause care in Primary Care settings:
- Provide funding for the Australasian Menopause Society to provide GP training about menopause
- Support GP’s at point-of-care through a combination of rapid-access specialist advice, practice software algorithms and streamlined referral pathways
- Ensure that GPs are well remunerated under Medicare for longer consultations, as recommended in the recent Strengthening Medicare Taskforce Report and the RACGP submission to the Senate inquiry into universal access to reproductive healthcare (7 Mar 2023)
To improve service access in rural and remote areas:
- Permanent inclusion of Telehealth items for reproductive and sexual health care in the MBS, as recommended in the RACGP submission to the Senate inquiry into universal access to reproductive healthcare (7 Mar 2023)
To improve access to information:
- We need public awareness campaigns which are accessible and easily understood regardless of education, language, gender identity, culture or disability.
- Provide funding for Australasian Menopause Society to extend its current range of online infographic, video, culturally adapted and translated resources.
- Funding for the development and maintenance of a DHAC website that collates all the best menopause resources for GP’s and consumers in one well-known, up to date location. Promote it via public awareness campaigns, Primary Health Networks and General Practice organisations.
To reduce the burden of suffering and chronic disease everyone needs to know about the menopausal transition: how it might impact their functioning and relationships, what lifestyle changes to make, how to manage symptoms and where to get support.
Everyone has the right to this information and access to appropriate, affordable services and treatment.
[NOTE: In this document “women” refers to people born with functioning ovaries, who will therefore experience menopause]
What is WellFemme About?
If you can’t find the professional help you need for your menopause or perimenopausal symptoms then book a Telehealth consultation with an expert WellFemme menopause doctor.
WellFemme is Australia’s first dedicated Telehealth menopause clinic, servicing locations nationwide including: Melbourne, Sydney, Adelaide, Darwin, Perth, Hobart, Brisbane, Dubbo, Bendigo, Broken Hill, Broome, Alice Springs, Launceston, Cairns, Mildura, Lightning Ridge, Kalgoorlie, Albany, Toowoomba, Charleville, Port Headland, Katherine, Ballarat, Coober Pedy, Bourke, Albury… and your place! 🙂
Tags
Dr. Kelly Teagle, menopause advocacy, menopause matters, parliamentary round table, Perimenopause,
Intimacy issues can be a lonely road. We tend to keep problems in this area to ourselves, not realising that many others are also suffering in silence.
Click above to watch our webinar: “Menopause and Intimacy”.
What’s “Normal”?
Let me reassure you that most women will experience sexual problems at menopause. In that sense, abnormal is actually… normal! For example:
- 75% of menopausal report problems with vaginal lubrication.
- 28% report pain with intercourse.
- 15% have vaginal itching, irritation or pain.
- Women are 2-3x more likely than men to experience reduced libido as we age
- In 1/3 of couples, male sexual dysfunction is the primary issue. Causes include medications, mood disorders and erectile dysfunction.
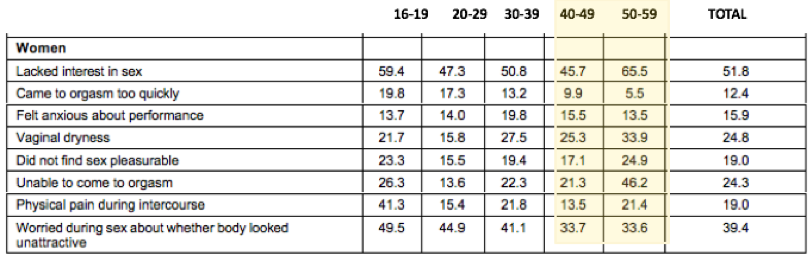
These figures are a little old, but the most frequently reported sexual issues in women aged 50-59 were:
- Lack of interest in sex (2/3)
- Inability to orgasm (almost half), and
- Equal third place were vaginal dryness and body image issues (about 1/3).
These seem like big problems right? Well they can be, if you let them. But remember, these issues are NORMAL at midlife and beyond. Once you realise that and stop worrying that there’s something wrong, you can get on with working out how to manage them. So here it is, my special gift to you, dear readers:
Kelly’s Deeply Insightful Solutions For The Commonest Sexual Problems At Menopause:
- Lack of interest in sex over 40 is… NORMAL. Only a problem if you fail to realise it and change your approach (more on that below).
- Difficulty orgasming. Also normal, but often unacceptable. Again a change of approach is required here, which can be tricky in a long-term relationship with very set routines and habits, but not impossible. Explore alternative means of stimulation, such as manual, oral or mechanical. The deep vibrations produced by some vibrators can really help speed up arousal and orgasm in postmenopausal women.
- Vaginal dryness can often be very successfully relieved with vaginal estrogen or testosterone and lubricants. Check out our resources below.
- Body image. Find your inner goddess (and/ or a more appreciative partner!). The table above proves that gorgeous young women are even more insecure than you, so clearly being young and gorgeous doesn’t solve the problem. Find what you/ your partner love most about your body and celebrate it. ShoulderFest perhaps? Break out the tank tops…
What Physical Changes Contribute To Sexual Problems At Menopause?
- Less estrogen results in lower vaginal blood flow and lubrication, tissue thinning
- Vaginal tissues are drier and more prone to pain and damage
- Less acid vagina, more prone to infection
- Ageing= lower testosterone= reduction in sex drive and responsiveness
- Hot flushes and mood changes make us feel tired, irritable, anxious or depressed… not sexy!
What Psychosocial Factors Are Contributing to Sexual Problems At Menopause?
- Quality of relationship with partner
- Grief/ loss: children leaving home, ageing or dying parents
- Prior levels of sexual satisfaction
- Emotional wellbeing
- Stress, eg. work, family dysfunction
- Past trauma, or guilt/ shame about sex
- Poor body image
What Other Factors Might Be Contributing?
- Poor general health
- Chronic pain or diseases
- Thyroid problems
- Menstrual problems, PMS
- Other conditions causing painful sex, like endometriosis, prolapse, infections
- Medications: particularly antidepressants
What’s Up With My Libido?
This depends what you mean by “libido”. Which of these applies most to you?
- I don’t feel like initiating or agreeing to sex much, but I can enjoy it once we get into it, and perhaps even orgasm.
- I don’t enjoy sex at all: it’s painful/ traumatic/ upsetting. I can’t get excited, lubricated or orgasm.
These are very different situations demanding a very different approach. I recommend you read Dr Rosie King’s wonderful book “Where did my libido go?” for a full rundown of the different categories of libido issues and their possible solutions.
The second situation does require investigation and management by a doctor and/ or therapist. The first however is very manageable if a couple is committed to communicating and working together to improve things.
Excerpts from Jean Hailes’ excellent “Libido” factsheet:
Health
- Maintain a healthy lifestyle: physical activity, a healthy diet, reduce your alcohol intake.
- Find ways to reduce stress and take time out to relax regularly.
Opportunity
- Create goodwill and some intimacy between you and your partner, by talking, listening and touching and holding each other, so you are more likely to feel sexual towards each other
- Don’t wait for sex to happen spontaneously – allocate time for sex
- Create a physical environment for sensuality and intimacy
Communication
- Let your partner know what makes you feel loved and encourage them to do these things and do the same for them in return
- Work with your partner as a team to deal with libido issues – if there is desire discrepancy try to find a compromise agreeable to both of you
- Communicate what works best for you during sex – your partner may not know what you like
Options. If you have low desire but still enjoy sex, try:
- ‘decision-driven’ sex rather than waiting to have ‘desire-driven’ sex – you make some decisions by saying to yourself: “Sex is good for our relationship, so even though I can’t be bothered, I will suggest making love tonight”
- sex for affection or intimacy or because sex is good for your relationship or because you enjoy sex
- manual or oral stimulation rather than intercourse
Realise that sex is not only penetrative intercourse but includes touching, kissing, holding, trusting and/or oral stimulation. Talk about this with your partner. Take it in turns to make love to the other with no expectations.
Exploration
- Rather than automatically saying no to sex when the opportunity arises, ask yourself “why not?” – if no good reason presents itself, give sex a try
- Optimise the quality of sex you are having with your partner – the better the sex, the more likely you are to want it
- Explore your own sexuality – get to know your sexual anatomy, learn how things work and what gives you pleasure
- Where do you like to be touched, what sort of pressure, can you bring yourself to orgasm? If you don’t know, how can your partner know?
- Nothing gives most men more pleasure than seeing their partner enjoy sex
- When together, focus on your own pleasure – stay present and enjoy
Chronic or long-term, low libido can create differences in sexual desire in couples. Sometimes, your partner can fear hurting you (physically and emotionally) and this starts a negative cycle in your sexual relationship.
The Pelvic Floor and Sexual Pain
Pelvic floor physiotherapist Marita O’Shea joined me on our live Webinar and gave an excellent presentation. Check out the video below to learn about:
- What the pelvic floor is and how relates to the vulva, vagina and pelvic organs
- Various causes of painful sex, and
- How you can manage sexual pain, dryness and other issues.
For further information about sexual pain you can also check out my Blog post “Love Hurts”. It contains advice about how to conduct your own self-assessment, by asking yourself:
- How old am I?
- Where is the pain?
- When does it happen?
- Have I ever had pain-free sex?
- Is there anything that looks/feels different? and
- Any other symptoms/ medical conditions?
You may get a pretty good idea of what’s going wrong from doing this, but should always consult with a trusted women’s health specialist for confirmation and treatment.
Resources
The Australasian Menopause society’s information sheet “Sexual difficulties in the menopause”: https://www.menopause.org.au/hp/information-sheets/722-sexual-difficulties-in-the-menopause
Jean Hailes resources about menopause and sex: https://www.jeanhailes.org.au/health-a-z/menopause/sex
Their “5 things to know about sex in later life: https://www.jeanhailes.org.au/resources/five-things-to-know-about-sex-in-later-life
Their Libido factsheet (I HIGHLY recommend): https://www.jeanhailes.org.au/health-a-z/sex-sexual-health/libido
Also their “Vulva and vagina” factsheet: https://www.jeanhailes.org.au/resources/vulva-vagina-fact-sheet
Where to buy vaginal dilators: https://pelvicfloorexercise.com.au/
How to use vaginal dilators: https://pelvicfloorexercise.com.au/resources/downloads/how-use-your-vaginal-dilators and https://www.pelvicexercises.com.au/vaginal-dilators/
How to know which lubricant to use: https://www.pelvicexercises.com.au/best-lubricant/
Or this guide from Sexual Health and Family Planning ACT
Pelvic floor relaxation and stretches: https://www.pelvicexercises.com.au/pelvic-floor-relaxation-stretches/
How to find a pelvic floor physiotherapist: https://choose.physio/find-a-physio
Mayo clinic- changing female libido- 5mins: https://www.youtube.com/watch?v=xDG4c5l0Y1I
Joan Price on sexuality for seniors- 40mins: https://www.youtube.com/watch?v=nIILHh1zPKE
Bliss for women free downloads: https://www.blissforwomen.com/collections/eswell/Download
_______________________________________________________________________________________________________________________________________________
What is WellFemme About?
If you can’t find the professional help you need for your peri/menopausal symptoms then book a Telehealth consultation with an expert WellFemme menopause doctor.
WellFemme is Australia’s first dedicated Telehealth menopause clinic, servicing locations nationwide including: Melbourne, Sydney, Adelaide, Darwin, Perth, Hobart, Brisbane, Dubbo, Bendigo, Broken Hill, Broome, Alice Springs, Launceston, Cairns, Mildura, Lightning Ridge, Kalgoorlie, Albany, Toowoomba, Charleville, Port Headland, Katherine, Ballarat, Coober Pedy, Bourke, Albury… and your place! 🙂
Tags
adelaide, australia, Early menopause, early signs menopause, hot flashes, Low libido, low sex drive, melbourne, menopausal symptoms, menopause, new south wales, northern territories, pain with intercourse, Pain with sex, Perimenopause, perth, Queensland, South Australia, sydney, Tasmania, vaginal dryness, vaginal pain, victoria, WellFemme, Western Australia,
